- Home›
- Healthy Living›
- 6 Common Female Urologic Conditions And How To Treat Them
6 Common Female Urologic Conditions And How To Treat Them
By: Priyanka Maheshwari Sun, 04 Feb 2024 2:55:30

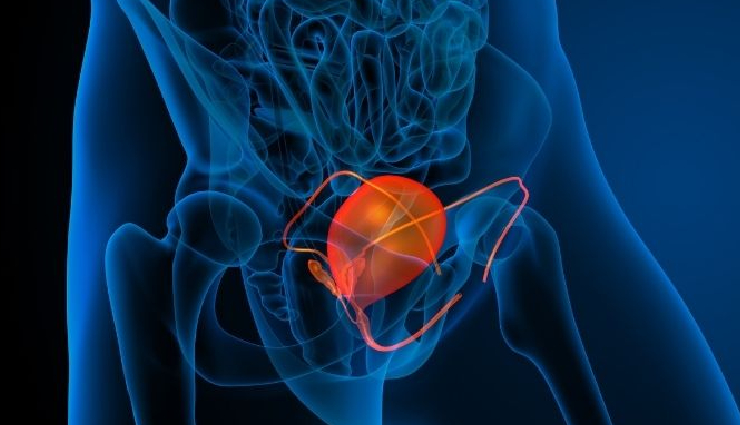
The urinary tract system comprises the kidneys, ureters, bladder, and urethra. Urology, a medical specialty, is dedicated to diagnosing and treating conditions related to the urinary tract and the male reproductive system. Urologists undergo training to address various issues and diseases, such as urinary tract infections, urinary incontinence, prostate cancer, kidney stones, and erectile dysfunction. Their expertise extends to conditions affecting male reproductive organs like the testes, prostate, and penis. Despite the misconception that urologists cater exclusively to men, female urology specifically focuses on diagnosing and treating urinary tract disorders and conditions that primarily or disproportionately impact women. This overview will explore common issues in female urology and their treatment approaches.
Several factors contribute to the heightened risk of specific urologic conditions in women. These factors include anatomy, hormonal fluctuations, sexual activity, pregnancy and childbirth, and lifestyle choices.
* Anatomy - The female urinary tract, being shorter and wider than the male tract, is more susceptible to infections. Additionally, the proximity of the urethra to the anus increases the risk of bacterial contamination.
* Hormonal Changes - Fluctuations in hormones during pregnancy, menopause, and various life stages can impact the urinary tract, elevating the risk of certain conditions.
* Sexual Activity - Women engaging in sexual activity face an increased risk of urinary tract infections due to the introduction of bacteria into the urethra. Maintaining good hygiene and urinating before and after sex can help mitigate this risk.
* Pregnancy and Childbirth - The physical changes in the pelvic area during pregnancy and childbirth may lead to conditions like urinary incontinence or a heightened susceptibility to urinary tract infections.
* Lifestyle Factors - Certain lifestyle choices, such as smoking and obesity, can amplify the risk of urologic conditions in women. Fortunately, modifying these lifestyle factors can contribute to preventing or reducing the likelihood of developing common urologic conditions.
Common Female Urologic Conditions and How to Treat Them

# Urinary Tract Infections
A urinary tract infection (UTI) is an infection occurring in any part of the urinary system, encompassing the kidneys, ureters, bladder, and urethra. Bacteria are the primary cause, with bladder infections (cystitis) being the most prevalent type. UTIs can also manifest in the upper urinary tract, such as the kidneys (pyelonephritis). Women face a higher risk due to anatomical factors and the proximity of the urethra to the anus. Preventive measures include maintaining proper hygiene, wiping from front to back, and urinating before and after sexual activity.
Common UTI symptoms encompass:
- Strong, persistent urge to urinate
- Burning sensation during urination
- Frequent, small amounts of urine
- Cloudy, dark, bloody, or strong-smelling urine
- Lower abdominal or back pain or pressure
- Fatigue or shakiness
- Fever or chills (indicating potential kidney involvement)
Treatment typically involves antibiotics to eliminate the infection. Following the full antibiotic course, staying hydrated aids in flushing out bacteria and alleviating symptoms. Untreated UTIs can lead to severe complications, such as kidney problems, sepsis, and septicemia.
# Overactive Bladder (OAB)
Overactive bladder (OAB) is characterized by a strong, urgent need to urinate frequently, often accompanied by a feeling of inability to retain urine, leading to urinary incontinence. Various factors, including nerve damage and bladder muscle issues, can contribute to OAB.
OAB symptoms include:
- Sudden, strong urge to urinate
- Frequent urination, often exceeding eight times daily
- Immediate need to urinate, sometimes resulting in leakage before reaching the bathroom
- Nighttime awakening for urination (two or more times)
Treatment options involve pelvic floor muscle exercises, medications to relax the bladder and reduce urination frequency, bladder training, Botox injections, nerve stimulation, and more. Consulting with a urologist or urogynecologist is crucial for accurate diagnosis and tailored treatment plans.

# Interstitial Cystitis
Interstitial cystitis (IC), also known as painful bladder syndrome (BPS), is a chronic condition causing discomfort or pain in the bladder and pelvic region, accompanied by an urgent and frequent need to urinate. The exact cause remains unknown, but it is thought to be linked to issues with the bladder lining, allergic reactions, or underlying immune system problems.
IC symptoms include:
- Urgent need to urinate
- Pelvic discomfort or pain
- Burning sensation during urination
- Pressure or tenderness in the bladder or pelvic area
- Frequent urination in small amounts
- Nighttime urination
Diagnosing IC is challenging, often involving the elimination of other potential conditions. Treatment options encompass medications, bladder instillations, nerve stimulation, physical therapy, pelvic floor exercises, lifestyle modifications, and more.
# Urinary Incontinence
Urinary incontinence (UI) is the involuntary leakage of urine, impacting individuals of all ages. Women are often disproportionately affected, primarily due to factors like pregnancy, childbirth, and menopause. UI includes stress, urge, mixed, and overflow incontinence.
Types of UI:
- Stress Incontinence: Leakage during physical activities or movements that exert pressure on the bladder.
- Urge Incontinence: Sudden, strong urge to urinate leading to leakage, often associated with an overactive bladder muscle.
- Mixed Incontinence: A combination of stress and urge incontinence.
- Overflow Incontinence: Leakage due to an overly full bladder unable to empty completely.
Treatment options, both surgical and non-surgical, include pelvic floor exercises, bladder training, medications, nerve stimulation, and surgical procedures. Seeking advice from a urologist helps determine the most suitable treatment based on the type and severity of incontinence.

# Postpartum Urinary Incontinence
Postpartum urinary incontinence, exclusive to women after childbirth, results from physical changes during pregnancy and childbirth, along with hormonal fluctuations. The pressure exerted on pelvic muscles during pregnancy and potential damage during childbirth contribute to this condition. Treatment aligns with non-pregnancy-related incontinence solutions.

# Pelvic Organ Prolapse
Pelvic organ prolapse (POP) occurs when supporting muscles and ligaments weaken or stretch, causing pelvic organs like the bladder, uterus, or rectum to descend into the vaginal canal. Pregnancy, childbirth, menopause, and increased pelvic muscle pressure contribute to POP. Symptoms include vaginal bulging, difficulties with bowel movements or urination, lower back pain, and vaginal bleeding or discharge. Treatment involves pelvic floor exercises, hormone therapy, pessary insertion for organ support, or surgical repair.





